Abstract
Background: Patients with active malignancy are frequently admitted to intensive care units (ICUs) and experience organ failure including acute respiratory distress syndrome (ARDS). In ARDS clinical trial populations, two immune phenotypes have been identified which seem to differ based on plasma protein expression, predicted mortality, and response to several randomized therapies. It is unknown if similar patters exist among ICU patients with hematologic malignancies as these patients are often excluded from clinical trials in critical care. We therefore sought to classify patients with leukemia who develop ARDS secondary to septic insult according to validated immune phenotyping algorithms and describe their characteristics and outcomes.
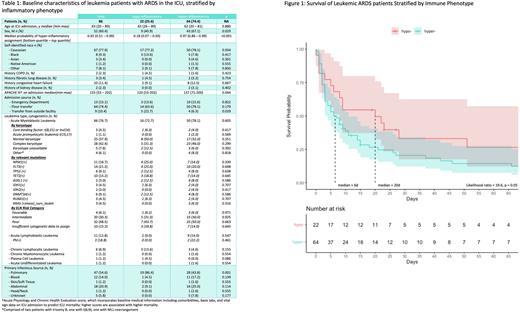
Methods: We conducted a prospective cohort study of sepsis subjects admitted to the ICU. Eligible patients had suspected infection and organ injury upon ICU admission; exclusion criteria included non-infectious causes of organ failure, a desire for comfort measures only, or lack of informed consent. Plasma collected on day 0 of ICU admission was profiled for proteins including IL8 and sTNFR1 by electrochemiluminescence. We limited our investigation to subjects with a diagnosis of active leukemia (acute or chronic) who developed ARDS (by Berlin criteria) within 6 days of ICU admission. Using a published parsimonious algorithm incorporating plasma IL8, sTNFR1, and bicarbonate, we assigned either a hyper- or hypo-inflammatory ARDS immune phenotype. We then constructed a multivariable Cox proportional hazards model controlling for APACHE III, history of BMT, sex, acute vs. chronic leukemia, and site of infection to assess the independent effect of phenotype assignment on mortality. Univariate comparisons between patients assigned to either phenotype were made as appropriate with T or Chi-Square tests.
Results: 86 subjects diagnosed with leukemia and ARDS between 2008 and 2017 were identified. In-hospital mortality was 76%. 64 (74.4%) were assigned a hyper-inflammatory phenotype using the 3-marker algorithm. Male sex, higher APACHE III, and non-pulmonary infectious source appeared to be associated with hyper-inflammatory assignment in univariate comparison, while tumor-specific characteristics such as leukemia type and cytogenetic features were not (table 1). Median survival in the hyper-inflammatory group was 6 days vs. 20 in the hypo-inflammatory group (log-rank p = 0.04, figure 1). However in our Cox proportional hazards model ARDS immune phenotype was not significantly associated with mortality (HR 1.63, 95% CI 0.87 - 3.08, p = 0.12). A sub-analysis of patients diagnosed with AML did not reveal any association between European LeukemiaNet cytogenetic risk category and mortality, controlling for the same baseline covariates and immune phenotype.
Interpretation: We identified previously described ARDS immune phenotypes among leukemic ARDS patients, though we did not observe an independent association between immune phenotype and mortality when controlling for relevant baseline covariates. At 76%, overall mortality was consistent with prior estimates in oncologic ICU patients and higher than the general population (~40%). A higher proportion of leukemia subjects were assigned to the hyper-inflammatory phenotype (74.4%) than described in non-oncologic trial populations (30-35% in 5 prior ARDS trials). Limitations include small sample size and knowledge that both malignancy and immunosuppression may affect cytokine expression such that phenotypic assignment is unreliable. Future efforts might focus on re-deriving ARDS phenotypes from a larger cohort of patients with hematologic malignancies in order to better understand how tumor interacts with the immunopathology of their critical illness.
Disclosures
Meyer:BioMarck Inc.: Research Funding; Endpoint Health Inc.: Other: consulting; Quantum Leap Healthcare Collaborative: Research Funding; Athersys Inc.: Research Funding.
Author notes
Asterisk with author names denotes non-ASH members.

This feature is available to Subscribers Only
Sign In or Create an Account Close Modal